Neonatal and Infant Mortality Rates Core Indicator
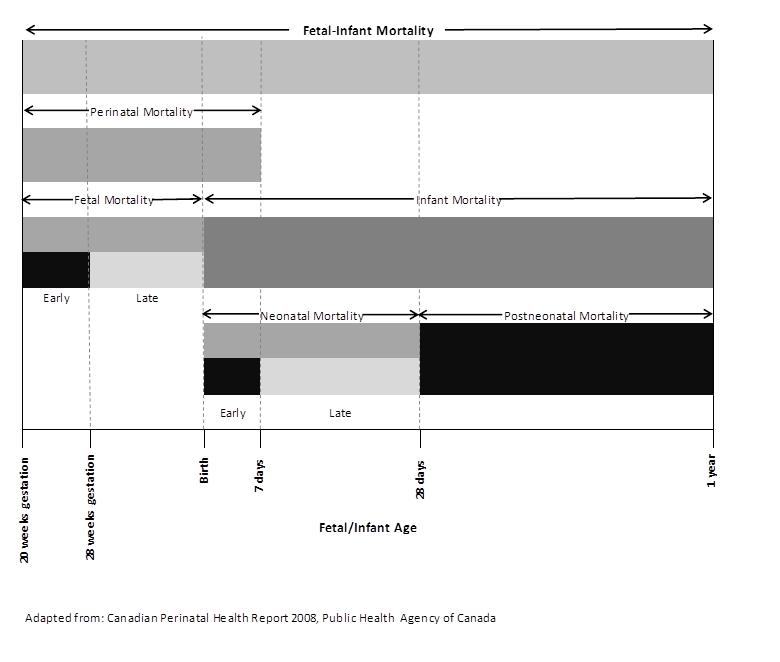
- The ratio of the number of deaths of live born infants during a calendar year per 1,000 live births in the same calendar year.
Method of Calculation
| Infant Mortality Rate Total number of deaths for live born infants (364 days or younger) 1000 Total number of live births 1000 |
| Neonatal Mortality Rate Total number of deaths for live born infants (27 days or younger) 1000 Total number of live births 1000 |
| Post-Neonatal Mortality Rate Total number of deaths for live born infants (28-364 days) 1000 Total number of live births 1000 |
Recommended Subset Analyses
| Age of Mother |
|
| Gestational Age |
|
| Birth Weight |
|
| Sex of Infant |
|
| Age of Infant |
|
| Geographic areas of patient residence |
|
Data Sources
|
Numerator |
Denominator |
Alternative Data Source(s) |
|
Original Source: Vital Statistics, Office of Registrar General (ORG), Service Ontario Distributed by: Ontario Ministry of Health and Long-Term Care (MOHLTC): IntelliHEALTH Ontario (IntelliHEALTH) Suggested Citation: Ontario Mortality Data [years], Ontario Ministry of Health and Long-Term Care, IntelliHEALTH ONTARIO, Date Extracted: [date]. |
Original Source: Vital Statistics, Office of Registrar General (ORG), Service Ontario Distributed by: Ontario Ministry of Health and Long-Term Care (MOHLTC): IntelliHEALTH Ontario (IntelliHEALTH) Suggested Citation: Ontario Live Birth Data [years], Ontario Ministry of Health and Long-Term Care, IntelliHEALTH ONTARIO, Date Extracted: [date]. |
None |
Neonatal Death ICD Codes
|
Classification |
ICD-10-CA |
ICD-9 |
|
All causes |
|
|
|
All accidental deaths |
V01-Z99 |
E800-E999 |
|
Homicide/infanticide |
X85-Y09 |
E960-E969 |
|
Shaken Baby Syndrome |
S06 with Y07 |
850-854 with E967 |
|
Child battery and maltreatment or criminal neglect |
Y06-Y07 |
E967 & E968.4 |
|
Falls |
W00-W19 |
E880-E888 |
|
RDS: Respiratory Distress Syndrome |
P22 |
769.0-769.9 |
|
SIDS: Sudden Infant Death Syndrome |
R95 |
798.0 |
|
Congenital anomalies |
Q00-Q99 |
740-759 |
|
Low birth weight (not short gestation) |
P05 |
764 |
|
Low birth weight with short gestation |
P07 |
765 |
|
Intrauterine hypoxia and birth asphyxia |
P20 & P21 |
768 |
|
Other conditions of the perinatal period |
P00-P04, P08, & P23-P96 |
760-764, 766, & 770-779 |
|
Pneumonia and influenza |
J10-J18 |
480-487 |
|
Certain gastrointestinal diseases |
A00-A09, K29, K50-K52, K55-K63 |
008-009, 535, & 555-558 |
Analysis Checklist
General Checklist
Vital Statistics - Mortality Data
- Use Deaths data source from the Vital Statistics folder in Intellihealth, select # ON Deaths measure (number of deaths for Ontario residents who died in Ontario). Note: deaths for Ontario residents who died outside the province are not captured in Vital Statistics.
- Select appropriate geography from Deceased Information folder. Include other items, depending on your requirements (ICD10 Chapter, Lead Cause Group, age group, sex, etc.).
- In the mortality data set, External Cause of Injury Codes (ICD10 V-Y; ICD9 E-Codes), and not Injury & Poisoning Codes (ICD10 S-T codes; ICD9 800-999 codes) are used in assigning primary cause of death.
Vital Statistics - Live Birth Data
- In IntelliHEALTH under Standard Reports, folder "01 Vital Stats", open " Birth Summary V2". This report summarizes information on births by age group and mother's residence (Ontario, PHU and LHIN). IntelliHEALTH also provides population data (total population, female population aged 15-49 years) for the calculation of rates. Refer to the Notes tab for information. Open tab "1.2 Births x PHU x Type x Age" to obtain public health unit data and tab "1.1 ON Births x Type x Age" to obtain Ontario data. The report can be modified, renamed and saved under your own folder or can be exported into Excel.
- The predefined report provides live birth and population data for the calendar years from 2000 to the most recent available. Table options can be edited to change the number of years of data presented. For years that are not displayed modify the calendar year filter to include the required years.
- The data contained in the Birth Summary V2 report includes birth to Ontario mothers in Ontario only.
- The notes section of the report provides important data caveats and background information on data sources and should be consulted.
[Additional Accordion to split up the Analysis Checklist]
- [Add bullets here - CAUTION: Right-click to "paste as plain text" instead of copy-paste. The web-editor pastes formats really strangely, and it's a mess to clean-up after the fact... ]
- [Press enter to get another bullet.]
[Additional Accordion to split up the Indicator Comments]
[Additional Accordion to split up the Indicator Comments]
References
Glossary
Cited References
Acknowledgements |
|
Lead AuthorsJessica Deming, Region of Waterloo Public Health Sandy Dupuis, Niagara Region Public Health Natalie Greenidge, Public Health Ontario |
ReviewersAhalya Mahendra, Public Health Agency of Canada (Core Indicators Work Group Member) Carmen Yue, Toronto Public Health |
Contributing AuthorsReproductive Health Sub-group |
|

Indicator Comments
General Comments