Perinatal Mortality and Stillbirth Rates Core Indicator
- Perinatal mortality: the total number of deaths of a fetus or infant between the end of the 20th week gestation and the end of the 6th day of life in a calendar year per 1,000 total births (live births and stillbirths) in the same calendar year.
- Crude stillbirth rate: the total number of stillbirths per 1,000 total births.
- Stillbirth rate ≥ 500 g: the total number of stillbirths ≥500 g per 1,000 total births.
Method of Calculation
| Perinatal Mortality Rate Total number of stillbirths and deaths in infants 6 days of age or younger 1000 Total number of births (live births & stillbirths) 1000 |
| Crude Stillbirth Rate Total number of stillbirths 1000 Total number of births (live births & stillbirths) 1000 |
| Stillbirth Rate ≥ 500 g Total number of stillbirths ≥ 500 g 1000 Total number of births ≥ 500 g (live births & stillbirths) 1000 |
Recommended Subset Analyses
|
Age of Mother Gestational Age Birth Weight Sex |
|
| Geographic Areas of Patient Residence |
|
| Specific Cause of Death |
|
Data Sources
|
Numerator |
Denominator |
|
Original Source: Vital Statistics, Office of Registrar General (ORG), Service Ontario Distributed by: Ontario Ministry of Health and Long-Term Care (MOHLTC): IntelliHEALTH Ontario (IntelliHEALTH) Suggested Citation: Ontario Stillbirth Data [years], Ontario Ministry of Health and Long-Term Care, IntelliHEALTH ONTARIO, Date Extracted: [date]. Ontario Mortality Data [years], Ontario Ministry of Health and Long-Term Care, IntelliHEALTH ONTARIO, Date Extracted: [date]. |
Original Source: Vital Statistics, Office of Registrar General (ORG), Service Ontario Distributed by: Ontario Ministry of Health and Long-Term Care (MOHLTC): IntelliHEALTH Ontario (IntelliHEALTH) Suggested Citation: Ontario Live Birth Data [years], Ontario Ministry of Health and Long-Term Care, IntelliHEALTH ONTARIO, Date Extracted: [date]. Ontario Stillbirth Data [years], Ontario Ministry of Health and Long-Term Care, IntelliHEALTH ONTARIO, Date Extracted: [date]. |
| Alternative Data Source | Alternative Data Source |
|
Original Source: Discharge Abstract Database (DAD), Canadian Institute for Health Information (CIHI) Distributed by: Ontario Ministry of Health and Long-Term Care (MOHLTC): IntelliHEALTH Ontario (IntelliHEALTH) Suggested Citation: Inpatient Discharges [years], Ontario Ministry of Health and Long-Term Care, IntelliHEALTH ONTARIO, Date Extracted: [date]. |
Original Source: Better Outcomes Registry Network (BORN) Ontario Distributed by: Better Outcomes Registry Network (BORN) Ontario Suggested Citation: BORN Information System [years], Date Extracted: [date]. |
Data Elements in the BORN Information System (BIS) Public Health Data Cube
|
Dimension |
Categories |
Data Dictionary Definition |
|
Pregnancy Outcome |
|
Stillbirth at >=20 weeks or >=500 gms |
|
Newborn DOB Calendar |
|
Newborn calendar year of birth |
Analysis Checklist
General Checklist
- Analyze mortality and live birth data by infant residence, not place of death. Analyze stillbirth data by mother's residence.
- Note that three data sources are listed for use: 1) Vital statistics, 2) Hospitalization, 3) BORN. The choice of data source will depend upon data quality within a health unit as well as data access and the specific analysis questions. Possible alternatives are provided in case the vital statistics are too far out of date.
- Please follow the Analysis Checklist for the selected data source(s). If using IntelliHealth, the Vital Statistics: Stillbirth page includes the relevant Analysis Checklist.
- When using hospitalization, please note that early neonatal deaths are well captured but later neonatal deaths will not be so well captured.
- There are some cautions when using BORN for this indicator. For instance, the definition of stillbirths in BORN can vary according to reporting source. The definition of neonatal deaths in the BORN data dictionary is <28 days, which is different from APHEO definition of <7 days. This difference may also affect reporting of stillbirths and perinatal deaths because perinatal deaths include stillbirths and early neonatal deaths.
Vital Statistics Live Birth Data
BORN Information System
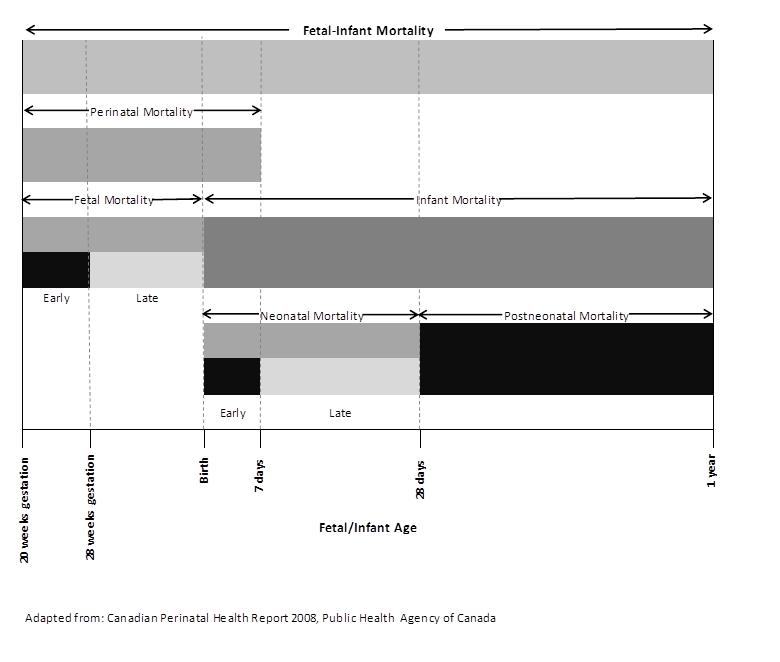
Components of Fetal-Infant Mortality
References
Glossary
Cited References
Acknowledgements |
|
Lead AuthorsAdam Stevens, Brant County Health Unit Natalie Greenidge, Public Health Ontario Carol Paul, Ontario Ministry of Health and Long Term Care Enayetur Raheem, Windsor Essex County Health Unit Nancy Ramuscak, Peel Public Health |
ReviewersSarah Ahmed, Toronto Public Health Reproductive Health Subgroup |

Indicator Comments
General Comments